Resources
Resources
Here you'll find new evidence and guidance from various sources across a variety of conditions of relevance to different audiences.
Resource
VR In The Workplace

Resource
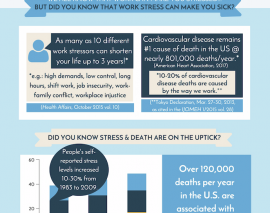
Healthy Work Agenda - Healthy Work Campaign

Resource
Study Summary: Complex Case Management and New Technology

Resource
Helping Men Decide on Prostate Cancer Treatment

Resource
A Patient Decision Aid to Help Heavy Smokers Make Decisions about Lung Cancer Screening
Resource
Enlisting the Brain in the Fight against Pain

Resource
Cancer in the Workplace - Supporting Treatment for Positive Employee and Employer Results
Resource
Identifying Personal Strengths to Help Patients Manage Chronic Illness
Resource
Can People Who Have Experience with Serious Mental Illness Help Peers Manage Their Health Care?